They shape you and you shape them. The talk between your immune cells and your bacteria can decide your shape.
Why do gut bacteria change? How can they make anyone fat?
Adapted from
Dancing mouse | CC0 1.0
Fat mouse by Clker-Free-Vector-Images | Pixabay
I have touched upon the topic of the gut microbiome (the bacteria that lives in your gut) earlier. I have talked about how they affect your metabolism. I have also discussed how the microbiome diversity is reduced in obesity and how it can contribute to type 2 diabetes. We have seen how bacterial community that lives in us can be shaped by our genetics, our diet and by the phycological stress we face. There are reports on how microbiome trains our immune system, affect our gene expression, and may even control our food cravings. However, what remains elusive is which microbial communities among the 1000s that live within us makes us obese vs which makes us thin. More importantly, what possible mechanisms could change the kind of communities that resides within us. In the paper I discuss today, the authors have discovered one such mechanism. They talk about how if the one kind of bacteria vs other dominates in our gut, it can cause obesity. They also discovered the role of T cells in regulating the type of bacteria that lives in the mouse gut.
The paper
The paper we will discuss today is titled T cell–mediated regulation of the microbiota protects against obesity published by Petersen et al., from June Round's and W. Zac Stephens' labs at Utah. It is published july 2019 edition of Science.
So how does the story start
Once upon a time, there were researchers working with germ-free mice. These are the mice born and brought up in a completely sterile environment and have never seen a bacteria in their life. Funny enough that even when these mice would eat a lot more food than their germ containing counterparts they would not gain any weight (Bäckhed et al., 2004). No, nothing at all. However, when they were given any germs to colonize their gut they would. If you gave them germs from obese humans they would even become obese. But when give them germs from lean humans, they won't gain as much weight (Turnbaugh et al.,). Moreover, one can take normal mice, treat them with antibiotics and give them either microbiome from obese or lean mice and alter how they gain weight (Ellekilde et al., 2014). In fact, it seems that in mice certain kind of bacteria is required in the gut for effective weight loss on a calorie-restricted diet (Wang et al., 2018). Now, all this is very interesting, it means there are some bacteria in the gut of obese humans that made them obese.
In fact, from sequencing microbes from obese individuals we know that there is reduction in the richness of their microbiome (Chatrlier et al., 2013). The species composition of obese and lean people show characteristic variations. Even if you were not looking at all the species in there, the overall functional profile of microbiome is different in obese vs lean individuals. For instance, gut bacteria in obese individuals are more potent in producing butyrate and other short-chain fatty acids, which are implicated in obesity (Chakraborti, 2015). Then, Zierer et al., 2018 gives a detail description of how age, sex and obesity can be correlated with differences in metabolites produced in the gut.
Anyhow, obese people have variant microbiome and all is fine. But the question arises that what changed this microbiome. Of course, there could be a genetic link to kind of microbiome you carry. It could also be your diet, your lifestyle, phychological stress, or just ageing that took the composition to the wrong turn (see my previous blog). Other than this the state of the immune system itself can alter the microbiome. From the day we were born our immune cells and gut microbes have been talking to each other. Now, imagine a situation where at some point in your life these talks get messed up. What if immune system because of age, stress or diet fails to keep a check on friends vs foes?
While on one hand obesity is associated with chronic low-grade systemic inflammation (see previous blog), on the other hand, obesity also makes us prone to some infections. In this regard, Tanaka et al., 1993 showed that T cell and B cell responses are compromised in obese individuals. Your B cells produce different classes of antibodies - IgG, IgM, IgA and IgE. Obesity is also associated with a reduction in secreted IgA levels in the gut mucosa. Though IgA deficiency in the gut doesn't have dire consequences it seems to have an effect on the composition and functional profile of microbiome (Pallaro et al., 2002, Fadlallah et al., 2018). It has been demonstrated in mice studies that IgA has a crucial role in the gut in maintaining healthy metabolism (Luck et al., 2019). Recently, it has also been shown that T cells carry toll-like receptors (these are the receptors that senses microbial patterns), which act through an adaptor protein called Myd88. This signalling is required for naive T cells to differentiate into T follicular helper cells (Tfh cells). Tfh cells signals B cells in lymph nodes of gut to start producing IgA. Perturbing this pathway by knocking out Myd88 in T cells causes dysbiosis in mice gut (Kubinak et al., 2014).
Nevertheless, what is not known is what is the mechanism by which the deficiency in Tfh cells affects IgA, change the microbiome and cause health consequences. This is what the current paper focuses on.
The story
Mice lacking a gene for Myd88 in T cells gains weight with age.
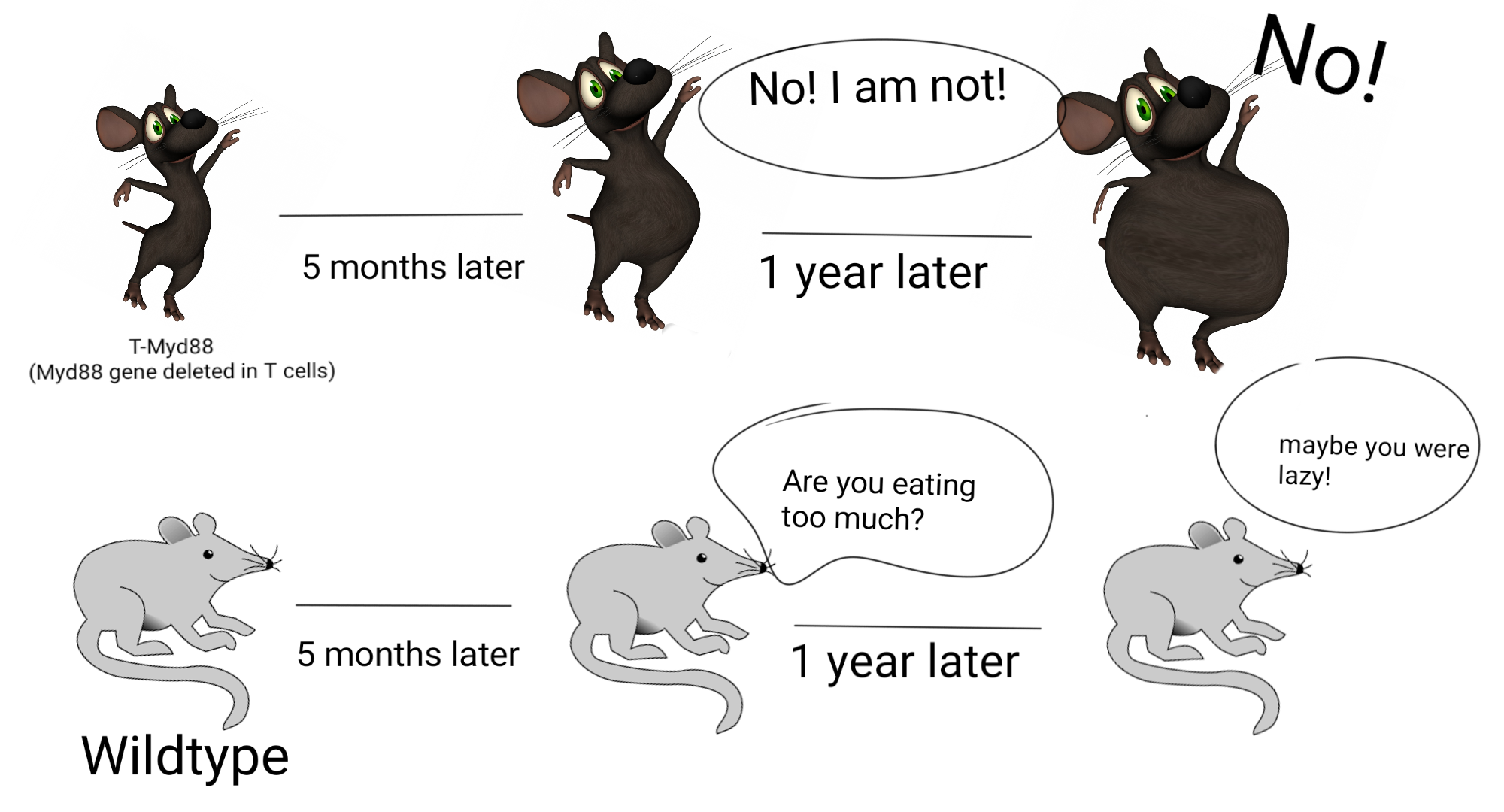
T-Myd88 mice (mice lacking Myd88 gene in T cells, gains weight over time. The wight gain is despite eating nothing more than wild type or being as active as wildtype. Illustrated by @scienceblocks using Image by da5id1 | public domain and Dancing mouse | [CC0 1.0].
The current story goes something like this. The researchers had a mouse which had Myd88 gene deleted specifically in T cells. They call it T-Myd88 mice. And the mice that have this gene intact, we are going to refer them as wildtype mice. The T-Myd88 mice seem to do fine for most of its life. But, hell breaks lose by the time it turns 5 months old. It starts gaining more fat. By the time its 1-year-old its at least twice as heavy as its wildtype cousins. It has at least 50% body fat percentage and a huge increase in visceral body fat. Oh, and it also develops obesity-associated fatty liver, chronic low-grade inflammation in adipose tissue and develops insulin resistance. Pretty much like obesity-associated pathology in humans.
T-Myd88's wildtype cousins perhaps tease it for eating too much or being too lazy. But guess what's funny. It ate the same chow as wildtype mice. In fact, at 2 months of age, it consumed a lot less food. By one year of age, it consumed no more calories than the wildtype guys. And to check whether these mice are being lazy, the researchers kept them in these special cages which can measure the metabolic activity of the mice by measuring its oxygen consumption. They also checked of these mice are moving around any less. But nada! They moved around as much as the wildtype guys. Though young mice showed slightly less energy expenditure, this difference did not persist as they grew older. So, neither the energy entering through the mouths of T-Myd88 nor the calories being burnt by it could explain the weight gain in these mice.
However, a lot happens between food entering the mouth and being burnt in the body. It matters how it is processed by the microbiome, how it is absorbed and how much of it is sent for storage vs consumption. Since T cells were knocked out a Myd88 gene, there could have been two explanations. Either the mutated T cell, by themselves, were changing the absorption of food or its storage, or they were indirectly doing so by interacting with the gut bacteria. It's a simple thing to test if its bacteria that is causing the weight gain then killing them by antibiotics in T-Myd88 mice should inhibit weight gain. And so it does.
Ok so now that they knew that it is most likely the bacteria that is making the T-Myd88 mice fat, the next question is how? Which bacteria is lost or gained? What functions are lost or gained? What are they doing? And what caused the loss or gain or these bacteria?
The war for colonization - Clostridia Vs Desulfovibrio
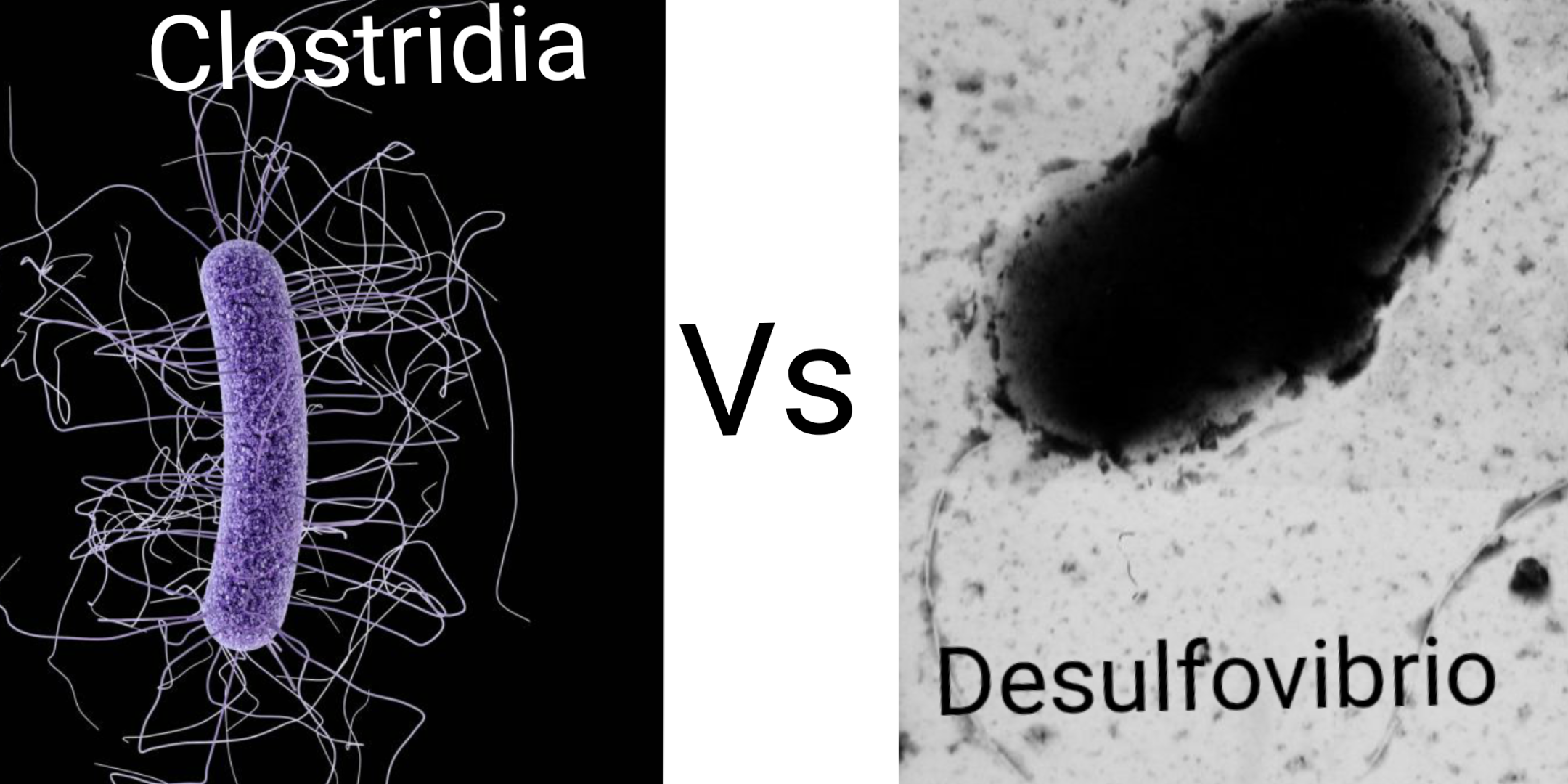
The genus Desulfovibrio seems to hate the class Clostridia. Clostridia by CDC/ James Archer | CC BY-SA 4.0. Desulfovibrio vulgaris by Graham Bradley | Public domain.
To know which bacterial species are lost or gained the authors sequenced the microbiome of T-Myd88 and wildtype mice. The authors did both 16S rRNA sequencing (that's ribosomal RNA to know the species details) and transcriptomics (to know the functional aspect by looking at gene expression). They found that there was an overall reduction in species richness in T-Myd88 mice. They also pinpointed that T-Myd88 have a reduced diversity of species and functions, esp relating to the class of bacteria called Clostridia
Communicable Obesity?
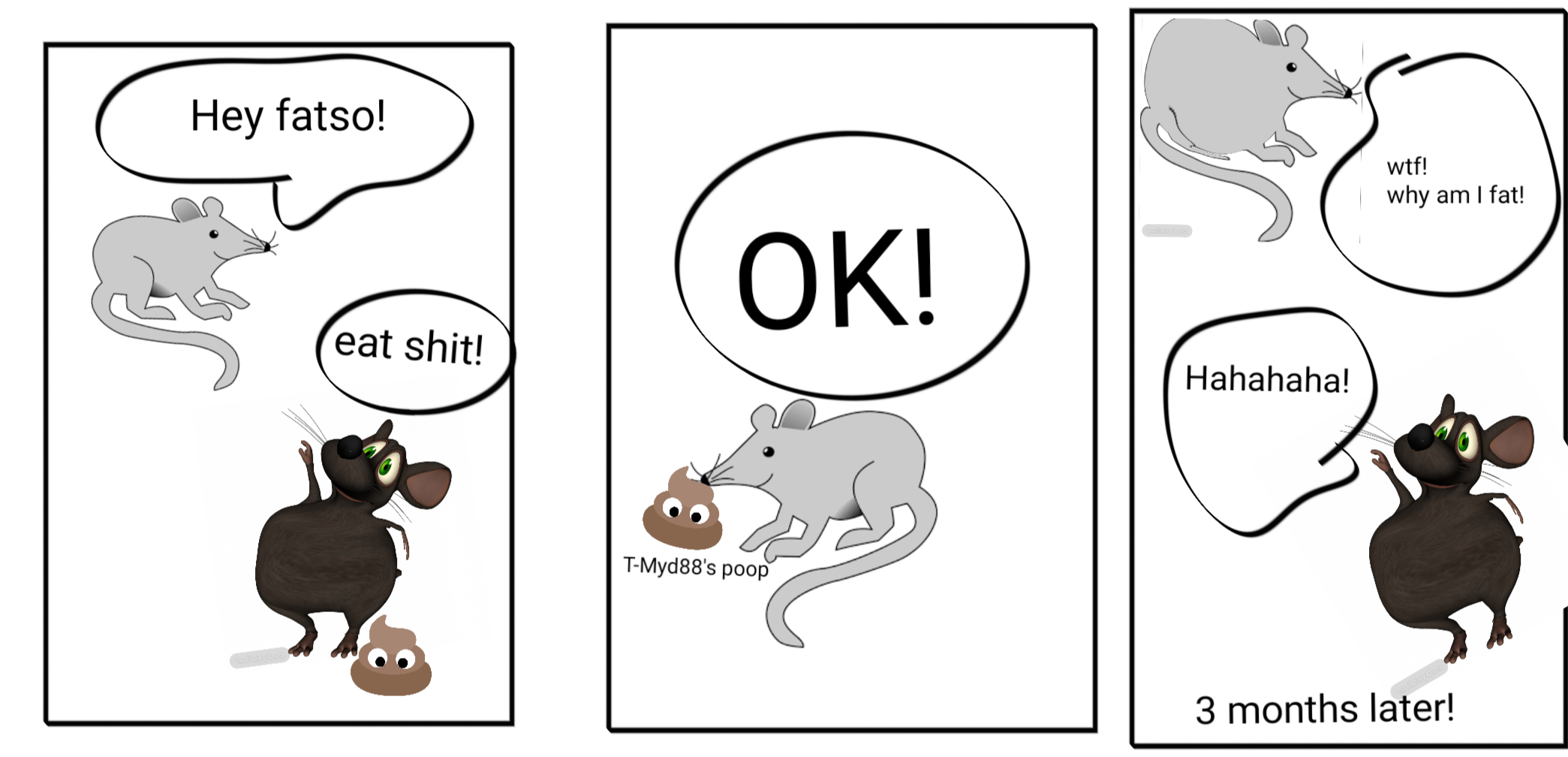
When wildtype and T-Myd88 mice were cohoused together, the wildtype mice became fat as well. Illustrated by @scienceblocks using Image by da5id1 | public domain and Dancing mouse | [CC0 1.0]. Poop by openclipart-vectors | Pixabay
Well, since mice literally eat shit, they hypothesized that if they keep wildtype and T-Myd88 mice in the same cage then they should be able to transfer their microbiome to each other's gut. This would either make T-Myd88 slim or wildtype fat. Well guess what, WT that stayed with T-Myd88 mice gained weight and their microbiome profile became similar to that of T-Myd88 mice. Which meant they too lost many species of class Clostridia.
And the winner is - Desulfovibrio
But here is the catch the microbiome of these two mice took 3 months to look similar, but the weight gain wildtype mice started as early as 3 weeks after starting a live-in with T-Myd88. So what was up with that? Seems like there was another bacterial family called Desulfovibrio that was first to take over the gut of partner wildtype mouse. So the authors thought that perhaps this is the guy responsible for making wildtype gain weight and also lose Clostridia over time. Desulfovibrio is the bacteria that degrade mucin (glycoproteins in mucous membranes) and produce hydrogen sulphide as a result. These sulphate reducing bacteria, which produce H2S and have also been found in the gut of humans with type 2 diabetes (Qin et al., 2012).
Hence, to test whether Desulfovibrio were sufficient to cause a reduction in Clostridia, they gave Desulfovibrio desulfuricans to pathogen-free wildtype mice. And there it was, 1 week later these mice lost some families and genus of class Clostridia. Then to further confirm of the loss of Clostridia is a direct effect of Desulfovibrio, authors colonized guts of germ-free (GF) mice (remember that GF mice have nothing in their gut, to begin with) with Clostridia and then gave them Desulfovibrio. And they were right, Desulfovibrio hates Clostridia. However, if they were right then giving fresh Clostridia to T-Myd88 mice should stop them from gaining weight. And, it does.
So why does Clostridia helps in keeping the mice lean and why does Desulfovibrio make them fat? Well maybe because some bacterial products leak into the gut of T-Myd88 mice that does not leak in wildtype? What could those products be? Maybe some inflammation causing products? But authors did not find a difference in this regard between wildtype and T-Myd88 mice. Moreover, anti-inflammatory drugs did not rescue weight gain in these animals. However, what authors did find is that T-Myd88 mice did show a difference in gene expression for genes involved in lipid metabolism and lipid absorption. Of these genes, the most interesting was the CD36 gene in the gut epithelium. This gene in gut epithelium downregulated by Clostridia, while Desulfovibrio upregulated its expression. The increased expression of CD36 caused long-chain fatty acids to pass through gut epithelium with ease. Hence, the weight gain in T-Myd88 mice can be blamed on increased absorption of long-chain fatty acids from the gut.
However, at the moment it is not clear which property of long-chain fatty acids is causing obesity. Is it just caloric value of these fatty acids or they also influence fat storage and metabolism in some way. I guess time would tell.
It all started with the T-cells
So far so good. But what is the evidence that T cells have any role to play in it? I mean sure, that the obesogenic microbiome arose in T-Myd88 mice. But does it mean that T-cells are required for maintaining healthy microbiome? Does the lack of properly functioning T cells favourable to the persistence of microbiome associated with obesity?
Well, normal T follicular helper cell and B cell interaction are important for proper IgA production that targets the correct bacteria. The hint for this comes from the experiment in which authors inject T helper cells from either wildtype mice or Bcl6 knockout mice into TMyd88 mice. Bcl6 knockout T cells can't differentiate into Tfh cells, and therefore can't educate the B cells to produce IgA. But T helper cells from wildtype mice can. The authors show that injecting wildtype T cells rescues weight gain in TMyd88 but injecting T cells from Bcl6 knockout background does not.
To test how microbiome is affected by T-cells authors took the Tcrb knockout mice (Let's call it TcrbKO). The mice lacking this gene, do not make T cells whatsoever. They killed the original microbiome of TcrbKO mice with antibiotics and then gave it 1:1 mixture of wildtype and T-Myd88 microbiome. They then injected them with T-cells, either from wildtype mice or from T-Myd88 mice. The mice that got T-cells from T-Myd88 mice gained much more weight. They also saw that only 10% of the microbiome received by TcrbKO mice was coated with IgA. But when they were given wildtype T cells >40% of microbiome got coated with IgA antibodies. However, IgA coating only increased to some 30% in mice receiving T cells from T-Myd88. Over the course of time, TcrbKO mice tha